Families prone to melanoma: a newly recognised familial melanoma gene BAP1
A newly recognized melanoma gene called BAP1
Some people inherit a genetic mutation (a section of altered DNA, which is the blueprint for the body), which increases their risk of cancer. In other words, this change in the blueprint for the body is passed on by a parent to his/her child and renders the child more susceptible to cancer later in life.
Usually these changes only increase the risk slightly. More rarely, people inherit genetic mutations which increase the risk of cancer considerably; these are known as “high risk” genes. The most well known genes like this are the BRACA 1 and 2 genes, which increase the risk of breast and ovarian cancer.
Some of these rare high-risk genes increase the risk of melanoma of the skin. The most common are CDKN2A and CDK4 and there is information on these genetic mutations on this web site. Overall, among individuals with skin melanoma, about 2% of them have a mutation in CDKN2A or CDK4. Because mutations in these genes can be passed on through families and increase risk of melanoma, then families with several family members who have each had melanoma are more likely to carry one of these high risk rare genes. In recent years, mutations in other genes have been found to significantly increase melanoma risk. These genes include POT1 and TERT. There is also information about POT1 on the website.
This information is about a fifth gene called BAP1. BAP1 was first discovered as a gene which is commonly mutated in melanoma of the eye, (known as uveal melanoma). At first in 2010, the damaged DNA was found just in the tumours themselves but in 2013 in one person the mutation was found in the eye tumour and the blood so that it was recognized that this was an inherited mutation. Since then considerable progress has been made in understanding what inheriting a mutation in the BAP1 gene means for people, and this article describes what is known so far. However, as this melanoma gene has so recently been discovered to be a cause of melanoma in families, much remains unknown.
It is important to realize that inherited BAP1, POT1 or TERT mutations are very rare indeed even in melanoma patients.
Unknowns
- We don’t know how many people who have inherited the mutated gene will actually develop cancer or what type of cancer
- We don’t know yet exactly what screening is needed
- And we don’t know how to reduce cancer risks
BAP1 mutations in families and melanoma
Although we now know that inherited mutations in the BAP1 gene causes skin melanoma in families just as do the more common melanoma genes such as CDKN2A, there are some important differences.
- People who are born with a BAP1 mutation develop unique-looking moles. Although these moles usually look harmless to the eye, under the microscope, these lesions can look like melanoma to the pathologist. Pathologists may use the term “spitzoid” to describe the appearance down the microscope.
-

Bapoma lesion on the scalp These “moles” are sometimes called “Bapomas” by medical teams looking after patients as they do seem to be quite distinct from more usual types of mole. They are typically 3-5 millimetres in size and look like shiny, small dusky red or orange bumps. In a way, they look like small mosquito bites, just deeper red in color. There is a difference though, mosquito bites disappear after a week or two, these spots persist forever. See picture opposite.
- The BAP1 spots can occur in the scalp and throughout the skin. It is not uncommon to have multiple spots develop (“crops” of spots).
- Although people with an inherited BAP1 mutation often have the pink Bapomas described above they can also get melanoma. Melanomas in BAP1 families may be unusual for melanomas, being more common on the scalp than usual. Although the melanomas have some characteristics seen in all melanomas, such as irregular colours and persistent growth they often arise deeper in the skin than usual and may not therefore have the classical features.
- It is also important to recognize that individuals who have a BAP1 mutation can also have other irregular looking moles besides the shiny red bumps.
- People who inherit the mutated BAP1 gene are at risk of melanoma of the skin but they are also at increased risk of other cancers. These cancers include the following:-
- Cancer of the kidney (renal cell carcinoma)
- Cancers of the lining of the chest, called mesotheliomas. Mesotheliomas may be caused by exposure to asbestos but in BAP1 families we suspect that they can occur even when there has been no exposure to asbestos
- Melanomas of the eye (uveal melanomas)
- Benign tumours of the tissues around the brain called meningiomas
Diagnosing an inherited mutation in the BAP1 gene
The diagnosis is usually suspected on the basis of the family history. The medical staff would ask the family about who had developed a cancer, at what age and what type of cancer. The family tree below is not real but shows the type of family history which might be suspicious for an inherited BAP1 mutation.
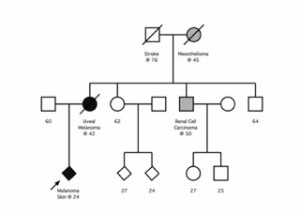 If a mutation was suspected then the family should be offered genetic counseling where an expert would review the family tree and if a BAP1 mutation was thought possible then a family member who has had a melanoma, particularly eye melanoma, might be offered gene testing. The availability and mode of testing varies between countries.
If a mutation was suspected then the family should be offered genetic counseling where an expert would review the family tree and if a BAP1 mutation was thought possible then a family member who has had a melanoma, particularly eye melanoma, might be offered gene testing. The availability and mode of testing varies between countries.
Normally gene testing is only carried out on a family member who has themselves had cancer, as a mutated gene is more likely to be found in such a person. The gene testing may take some considerable time to produce an answer because the tests are specialized and time may be required for additional tests to be sure that the change in the gene detected was a significant (harmful) one.
Screening
At the moment it is not clear what screening should be offered to family members with BAP1 mutations. With time, research will allow advice to be given on the basis of detailed data collection from families.
In the meantime clinical geneticists are likely to advise screening based upon what is known about BAP1 families and the person’s own particular family history. Having too many x-rays may also increase the risk of cancer so the medical teams seek to avoid too many scans whilst trying to scan frequently enough to detect cancer early.
Regular ultrasound examinations of the kidney would normally be suggested, an x-ray, low-dose spiral CT or MRI might be suggested for the chest (variable between health care systems), and less frequently body scans for those individuals who carry a BAP1 mutation.
Cancer prevention
We have no proof that lifestyle change will prevent cancer but it seems likely that this is so. It therefore seems sensible to suggest the following:-
- Engage in regular sun protection- this is a known risk factor for skin melanoma and is a good practice for prevention of all skin cancers in general.
- Avoid vitamin D insufficiency if sun avoidant or if you live in a temperate climate such as the UK.
- Avoid smoking, or stop as soon as possible
- Moderate alcohol intake
- Regular exercise as recommended for health generally
- Avoid obesity
- Avoid a diet heavy with meat
